Have you heard of breast implant illness? A few years ago, neither had I. But as the years went on, I had more and more symptoms related to breast implant illness including an autoimmune disease. Here’s my story of why I got my breast implants removed.
Why I Got My Breast Implants Removed
I never thought that I’d be “one of those” who wanted implants. To be honest, I was happy with my size – pre-kids, that is. Annnd then there were pregnancies and of course breastfeeding. I nursed my first two girls for 15 months each, and after doing so, my breasts showed it. I started to refer to myself as “National Geographic” – not a proud thing to admit, but it bothered me. I knew that I was slowly heading to “the other side.” I wanted to feel more like myself, to not look in the mirror and despise the stretched-thin bags of love. Little did I know that this was a pivotal moment in my life that would send me to numerous doctors, involve unexplained (and some explained) illnesses, and finally send me back to my starting point. Here’s my story of why I got breast implants and — spoiler alert — why i got my breast implants removed.
Why I got breast implants
When I first started noticing breast implant illness symptoms
To be honest, I never knew that I had any potential symptoms. I actually just assumed that since I had gone through another pregnancy that my body had again changed, causing some of the issues that I started having. After having three girls, we finally got our baby boy with our fourth child. And come hell or high water, I was going to nurse him for over a year, just like I had done with the girls. But things didn’t go that well. My production was nothing like it had been with the girls; he struggled to get what he needed when nursing. I felt guilty, sad, like a failure. How could I not do the same for him that I had done for the others? I had never used formula and I was convinced that I wouldn’t do it with him. But not only was my production low, I also immediately developed Raynaud’s Syndrome – in my nipples. Raynaud’s Syndrome is a vascular disorder that causes intermittent interruption of blood flow to the extremities. The affected body part (my nipples, in this case) turns white or blue and feels cold and numb. It was incredibly painful and tough to get circulation back. And it was NOT easy to work through. So instead I decided the next best option was to pump. I pumped and supplemented with formula for 15 months. Looking back, I’m sure that I damaged some breast tissue and I’m also not sure how smart this was given that I had implants.

2011 after the birth of our fourth and final child
Breast Implant Illness Symptoms
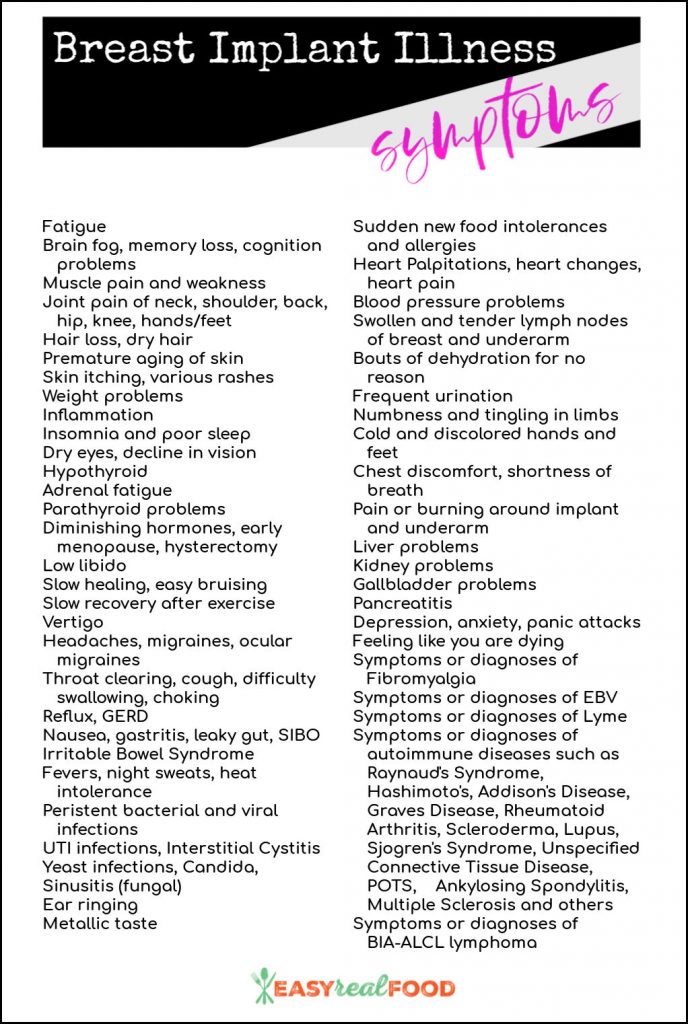
Below is a list of symptoms that are associated with Breast Implant Illness (BII). It took me two years to admit that I may in fact have BII. During that time, three different friends had directed me to the information out there on Breast Implant Illness. When I finally went through the list, I realized that I had 29 of the symptoms, including the following:
- Fatigue
- Brain fog, memory loss
- Muscle pain and weakness (more on this in the last symptom)
- Joint pain
- Hair loss
- Premature aging of skin
- Skin itching – I would break out into random itchy bouts.
- Inflammation – this went down immediately after explant surgery
- Insomnia/poor sleep
- Dry eyes
- Hypothyroid
- Low libido
- Slow recovery after exercise
- GERD
- Leaky gut
- Heat intolerance
- Persistent bacterial and viral infections
- Yeast infections
- Ear ringing
- MANY food intolerances (which spawned me to start this site!)
- Heart palpitations
- Swollen lymph nodes under breast
- Numbness and tingling in hands
- Cold and discolored hands
- Liver problems
- Gallbladder problems
- Panic attacks (just a few, but still noted)
- EBV
- Rheumatoid arthritis
My diagnosis over the past 11 years (during which had breast implants) include:
- Raynaud’s syndrome
- Mast cell activation disorder
- Hypothyroid
- GERD
- At risk for primary biliary cirrhosis
- Epstein Barr Virus
- Rheumatoid arthritis
- Probable celiac (I’ve been gluten free for so long that they can’t adequately test me)
Studies done to further validate breast implant illness
While Breast Implant Illness is not currently recognized as a medical diagnosis, the Food and Drug Administration and other major health authorities have been giving it more attention recently. In May 2019, the FDA released a statement noting that the agency’s officials are “taking steps to better characterize BII and its risk factors, and are considering ways to help to ensure women have all of the information they need to make informed decisions about whether to obtain breast implants or to remove existing breast implants in an effort to reverse systemic symptoms.” In October 2019, the FDA put out a recommendation for manufacturers to include a black box warning on the packaging of implants along with patient information to be included in a booklet that patients receive.
Research that supports the validity of Breast Implant Illness:
- MD Anderson did a study that shows an association between silicone breast implants and rare diseases.
- This study by the Natural Center for Health Research is eye-opening as well. It shows the improvement of symptoms following breast implant removal.
- There was an association with breast implants and autoimmune/rheumatic diseases discovered through this study as well.
Should I get my breast implants removed?
- Your saline implants have deflated.
- Your silicone implants have ruptured.
- You’ve developed capsular contracture.
- Your breasts are asymmetrical or deformed.
- You want to change your implant size.

What to expect when getting breast implants removed
- I’d be remiss if I didn’t mention that there is an emotional journey following explant surgery. I was not prepared for this. Sure, I knew that I’d look different – but I was in a funk for weeks afterwards. Some people bounce back right away, but I mourned the loss of something that I had. My body was different, and it took getting used to. A LOT of it.
- Explant surgery is a big deal, and everyone’s reaction is different. You may feel good right away, or it may take you weeks to get back to normal. What I can suggest is patience, giving yourself grace, and allowing yourself the time to heal, both physically and emotionally.
- While your surgeon will give you specific instructions, for the first two weeks my surgeon requested I not move my arms from my sides. Basically you can use from your elbows down, but that’s it.
- For the first six weeks post op, you cannot push, pull or lift anything over five pounds. I was grateful that I had my surgery during quarantine and had my family at home to help with daily tasks.
- As each surgeon has their own protocol, they will be able to give you specific instructions on best practices that they suggest.
- Breasts will change with time after explant. After doing a lot of research, I did find a physical therapist who helped with scar tissue and range of motion. I also practiced cupping, which is an ancient form of alternative medicine in which a therapist puts special cups on your skin for a few minutes to create suction. I went to a therapist at first, but also practiced it daily myself. Cupping is said to help with pain, inflammation, blood flow, relaxation and well-being, and as a type of deep-tissue massage; I had a slight adhesion on my left breast, and was trying to work that out with cupping in addition to encouraging blood flow to the area.
Products that helped me during/after explant
- This pregnancy pillow was very helpful in not allowing me to roll onto my side. My surgeon suggested sleeping on my back for 6+ weeks, so I definitely made good use of it.
- These bras were instrumental post surgery.
- Having hoodies that zip up is important. I wore them for the first three weeks following explant surgery.
- As mentioned above, I began cupping at three weeks. I used this cupping set that was recommended to me.
- If you also choose to cup, it is suggested to use fractionated coconut oil with it to help the cups move.
- A journal can be helpful. It was an emotional journey, and I found that journaling was incredibly helpful.
- Keeping hydrated is key. I tried to keep a straw cup nearby at all times to ensure that I was drinking enough water.
- If you have to take antibiotics with your surgery (I did not) and battle yeast infections, or if these have been an issue of yours with implants, this is the best candida remedy that I’ve found.
Getting your breast implants removed is a very personal decision. I know that at this point, even three weeks out from my surgery, I’m glad that I did it. I’ll post an update in six months to let you know how I’m feeling, but knowing that I have removed them from my body gives me peace. If you have any questions that you’d like to ask me directly, please feel free to reach out. I’d be happy to help and be a sounding board if I can.
All included information is not intended to treat or diagnose. The views expressed are solely mine and should be attributed as such. For medical questions, please consult your healthcare provider.









Wow, that’s a remarkable story. Very brave of you to share it. I hope your body totally heals and your story helps others that might be struggling with the same decision.
Thanks so much, Joni. Definitely took some deep breaths to put this out there, but am hoping that it can help others. ????
You are beautiful, this story is intense. I want mine removed but I can’t afford it and yet they are literally killing me. I have scleroderma Moravia. I’m genuinely scared to die. Things I wish I knew beforehand these death bags should come with warnings
Thank you, and I’m so sorry. So many of us living with varied conditions. Things we didn’t know:(. Please feel free to email me directly if I can help be an ear to listen. ❤️❤️
Thank you for sharing your story! I am 3 weeks post-op, and I too have an adhesion on one side. Just wondering if your adhesion ever released as a result of the cupping?
Cupping definitely helps as does fascia release with a trained massage therapist.
Wow, thank you so much for sharing your experience so far. I just ordered those bras. I’m 10 days post op explant + mastopexy. Both Allergan 410 implants from 2001 were ruptured. I had all kinds of BII symptoms in the last year…during Covid. I’m hoping things improve. I kind of overdid it today and am in some pain. So dumb. Gotta stop reaching and pulling. Can’t screw this up! So far the “cosmetic” portion (mastopexy) has set me back almost $14k. Not an easy pill to swallow. Btw, I tried to join that Facebook group you mentioned a few times and they just ignored me. Kinda disappointed since I had and still have lots of questions.
Oh gosh, of course! It’s been so nice to connect with others. It’s not a “fun” time, so it’s really wonderful if we can all support each other.
Please don’t overdo it. As they say; there is always tomorrow. You’ve been through a lot … give yourself time to rest and recover. 💕💕 Feel free to reach out anytime!!
I am 1 week post op myself. I had 15.5 year old mentor smooth saline under the muscle. Managed to nurse all 4 kids for a total of 12 years but my health was in steady decline. An explant, lift, and fat transfer set me back 17k. I am so angry that they didn’t present any of this information when I had my implants placed. I never would have done it. I literally poisoned myself with the assistance of a Surgeon which seems to go against their code of ethic of doing no harm. These should be illegal period!
I feel your frustration! It’s hard to not get angry about it … but honesty at 12+ months post-explant, I feel SO much better that I am trying to make peace with that. Best of luck with your healing!!
I have just had explant procedure three days ago its comforting to read these comments, already I have noticed an improvement.
How are you feeling ? How do they look?
I am getting my 11 year old saline, under muscle implants removed next month. I am only doing local anesthesia and removing them in the surgeon office. Did you have a full en-bloc to remove yours?
Thank you for your blog. I am 4 days post-op. I had a nightmare breast implant story of 4 revisions and finally found a MD that took them out. I acquired an extremely rare auto-inflammatory disease during my implants. I have a Team at Mayo and other specialists that have been following me. It’s been a horror story. I am taking antibiotics. I ordered the yeast product you mention.
I am praying that I get through this. A lot of pain.
I decided to start a blog. Nobody will believe the trauma I have endured these past decades of have these awful implants.
I’m now a size A/B? Hard to tell. But so happy the top out the 450cc’s the last MD put in when I asked for 300cc. I cried for weeks. And then the problems started and endless ED visits and near death twice.
UGH. I could go on and on. But too tired and tearful right now. Just grateful they are finally out of me.